🦵 Sciatica: From Back to Leg – A Sports Physio’s Breakdown
By Physiocure: The Sports Rehab Clinic, Santacruz (W)
What is Sciatica?
“Sciatica” is the term used when pain, tingling, or numbness travels from your lower back or buttock down the leg — following the sciatic nerve.
It’s not a disease but a symptom pattern caused by irritation or compression of the nerve or its root.
According to the National Center for Biotechnology Information (NCBI), sciatica typically arises from lumbosacral nerve root irritation, most commonly at L5 or S1.
👉 Source: NCBI – StatPearls
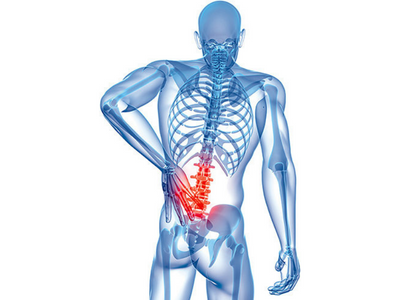
Anatomy of the Sciatic Nerve
The sciatic nerve is the largest and longest nerve in the body, originating from the L4–S3 spinal nerve roots within the lumbosacral plexus.
It exits the pelvis through the greater sciatic foramen, usually below the piriformis muscle, and travels down the back of the thigh before splitting into:
- Tibial nerve
- Common peroneal (fibular) nerve
It supplies:
- Motor control to hamstrings, most lower-leg and foot muscles
- Sensory input from the back of the thigh and leg to the foot
Variations in its pathway (e.g., passing through the piriformis) occur in 10–30% of people, sometimes leading to entrapment or nerve tension.
👉 Source: PMC – Sciatic Nerve Variations
👉 Source: Spine-Health – Nerve Anatomy
How Sciatica Develops?
Sciatica occurs when mechanical pressure or inflammation affects the sciatic nerve or its roots.
Common Mechanisms Include:
- Disc herniation or bulge: The soft center of a spinal disc presses on a nerve root.
- Spinal stenosis: Narrowing of the spinal canal squeezes the nerve.
- Piriformis syndrome: The nerve is compressed as it passes under or through the piriformis muscle.
- Inflammatory irritation: Chemicals released by injured discs increase nerve sensitivity.
- Biomechanical overload: Repetitive bending, twisting, sprinting, or sitting can increase lumbar stress.
Research shows both mechanical compression and inflammatory sensitization contribute to sciatic pain, altering nerve conduction and muscle activation.
👉 Source: British Journal of Anaesthesia
Why Does Sciatica Happen in Active People?
From a sports physiotherapist’s perspective, sciatica often develops from faulty movement patterns:
- Core or glute weakness
- Hip mobility restrictions
- Asymmetrical loading (e.g., one-leg dominant sport actions)
- Poor lifting or sprint technique
These factors cause uneven stress on lumbar discs and surrounding fascia, eventually irritating the nerve root.
Do You Need a Scan Before Seeing a Physio?
Not always.
Most cases can be clinically assessed without imaging. Your physio can diagnose sciatica using movement, posture, strength, and neural tension tests.
MRI or CT scan is only required if:
- Pain is severe or worsening
- There’s groin numbness or loss of bladder/bowel control
- Progressive weakness in the leg
- Symptoms last >6–8 weeks despite good therapy
Current clinical guidelines recommend early physiotherapy over early imaging in most cases.
👉 Source: NICE Clinical Guidelines – Low Back Pain & Sciatica (2024)
Rest or Physiotherapy — What Works Better?
Gone are the days of long bed rest.
Modern research clearly shows that prolonged rest slows recovery. Controlled, guided movement helps reduce inflammation, maintain mobility, and restore normal nerve motion.
A 2023 review found that early physiotherapy interventions improve function and reduce pain faster than inactivity.
👉 Source: NCBI – Early PT for Sciatica
✅ Short rest (1–2 days) if pain is severe
🚫 Avoid complete bed rest
✅ Start guided movement as soon as tolerated
Phases of Sciatica Recovery
1️⃣ Acute Phase (0–2 weeks)
Goal: Calm pain, reduce inflammation, and protect the nerve
Focus:
- Education and posture correction
- Gentle nerve mobility and decompression exercises
- Light core activation
2️⃣ Sub-Acute Phase (2–6 weeks)
Goal: Restore movement and strength
Focus:
- Hip and glute strengthening
- Controlled mobility
- Correcting movement faults
- Neural glides and flexibility
3️⃣ Return-to-Sport Phase (6–12 weeks)
Goal: Rebuild performance safely
Focus:
- Running mechanics, plyometric loading
- Core-hip integration
- Fascial line rehab (Superficial Back Line and Spiral Line work)
4️⃣ Maintenance Phase (beyond 12 weeks)
Goal: Prevent recurrence
Focus:
- Regular mobility and strength
- Load management
- Posture and ergonomic corrections
Latest Research-Based Treatment Trends (2025 Update)
| Technique | Evidence & Effectiveness |
|---|---|
| Neurodynamic (Nerve Glide) Exercises | Improve nerve mobility and pain modulation; supported by multiple RCTs. |
| Fascial Line-Based Rehab | Addresses kinetic chain imbalances; useful in athletes with recurrent sciatic symptoms. |
| Shockwave Therapy & Dry Needling | Moderate short-term relief for muscle-related sciatica; best as adjuncts. |
| AI-Based Movement Analysis | Helps identify asymmetry and reduce recurrence risk; emerging in elite rehab. |
| Pain Neuroscience Education & Mind-Body Training | Reduces central sensitization and improves recovery outcomes. |
Recent meta-analyses confirm that active rehab, neural mobilization, and patient education remain the most effective non-surgical interventions for sciatica.
👉 Source: Journal of Orthopaedic & Sports Physical Therapy (2024)
How Long Does Sciatica Take to Heal?
Most mild-to-moderate cases improve in 4–8 weeks with early, consistent physiotherapy.
Athletes with higher training loads may take longer due to repeated lumbar stress, but structured rehab minimizes relapse risk.
Final Word
Sciatica can be frustrating — but it’s highly treatable.
The best outcomes come from early physiotherapy, graded movement, and education.
At Physiocure, we focus on treating the root cause — not just the pain — so you can move, perform, and live pain-free.
📍 Physiocure: The Sports Rehab Clinic, Santacruz (W)
📞 Call: 9833072272
💬 Move Better. Heal Smarter. Perform Stronger.