Patellar tendinopathy is a common painful, overuse disorder, often presenting with knee pain in the front portion below the knee cap area.Also commonly known as Runner’s knee or Jumper’s knee. A thorough history and physical examination are necessary, but imaging can also aid in the diagnosis. The majority of cases resolve with physiotherapy. Once patients pass the initial inflammatory phase and remain symptomatic, treatment becomes more difficult.
Patellar tendinopathy is a common painful, overuse disorder, often presenting with knee pain in the front portion below the knee cap area.Also commonly known as Runner’s knee or Jumper’s knee. A thorough history and physical examination are necessary, but imaging can also aid in the diagnosis. The majority of cases resolve with physiotherapy. Once patients pass the initial inflammatory phase and remain symptomatic, treatment becomes more difficult.
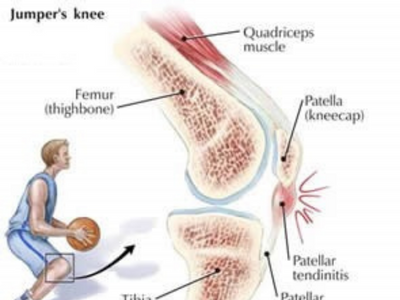
Let us first try to understand where the patellar tendon is.
On the front of the thigh a group of muscles called quadriceps are placed. These muscles form a tendon just above the knee cap (patella) which passes on and around the patella and extends to end at the shin bone (tibia). The portion below the patella is called the patella tendon
What is the function of this tendon?
- It connects the quadriceps muscle to the shin bone. Or it connects the thigh to the shin over the knee joint.
- Because of its structure it can transmit the force generated by this muscle as well as absorb ground reaction forces without minimal energy loss.
- It is flexible in nature.
- It provides proprioception- this means it provides constant signalling of the knee position to the brain and helps the brain respond appropriately.
What is the tendon made of?
- It’s made of collagen which can bear the load put on the tendon & elastin component which provides some flexibility to the tendon.
- This combination is arranged in several layers which then forms a guy rope kind of structure made of thin fibril like ropes assembled together.
- This guy rope is further covered by thin sheet of connective tissue called paratenon which provides nutrition to the tendon.
the more chronic or older your tendon problem will be the deeper it will reach to the tendon and may take a longer time to get the structural integrity back. but the best part is it is possible to restore the structural integrity with just physio
How does the tendinopathy develop?
- Tendinopathy means some pathology in the tendon.
- When the tendon is suddenly loaded beyond its capacity to handle, there is some damage to the minute structure within the tendon. If these structures are not able to recover appropriately, overall the tendon is not fit to even take the normal load leading to tendinopathy. This would be the sudden overload theory.
- Secondly if the tendon is repetitively loaded without sufficient time for recovery, slowly over a period of time the minute structures within the tendon are not able to take the load leading to the tendinopathy.
- Thirdly the quadriceps muscle force generation has an effect on the tendon. Is it is tight the force generated cannot be dissipated properly or if there is continuous eccentric load which the muscle can’t handle, then the tendon takes the beating.
The location where the tendon tends to develop a pathology?
Usually the tendon injury in detail is identified by its location that is, whether tendon is injured at its attachment on the knee cap, in the middle part of the tendon or at the lower portion attached on the shin bone is injured. The evidence based on a research below states the following
“This study confirms that patellar tendinopathy is not restricted to the proximal pole. Although the proximal pole was the most commonly involved location, distal pole involvement was common occurring in 38% of scans. The vast majority of previous studies have concentrated on proximal disease to the neglect of distal disease. Involvement of the mid patellar tendon was less common and when it did occur it almost always occurred in conjunction with pathology of either the proximal and/or distal poles. Isolated involvement of the middle portion of the patellar tendon was very rare (occurring in only one scan). As a result of this study the following recommendations are made:
This means that the tendon can get affected at the bone attachment near the patella or the shin bone, however getting injured in the middle part of the tendon is rare. Also the rehab program is different depending on the location of the injured tendon.
How does the tendon respond to loading?
When we talk about tendon loading, what we are discussing is repetitive jumping activities or exercises where the quadriceps muscle needs to be stretched and handle the body weight at the same time which directly loads the tendon. To understand how the pathology develops it is necessary what factors affect the loading of the tendon.
- If the tendon is thicker or longer it can with stand more load
- With age the load bearing capacity reduces and it takes longer time to recover.
- The tendon cannot withstand a situation where the tendon is getting compressed and loaded.
- It cannot withstanding loading continuously especially when it is fatigued
- If the leg has been immobilized for a long time, the tendons load bearing capacity reduces.
- The tendons microcirculation if impaired, it will affect the nutrition to the tendon and indirectly delay the healing, in that case again the tendon may not be able respond normally to normal loads.
- Local injection of corticosteroid into the injured tendon cause further thinning of the tendon and decreased strength, affecting the ability to bear load.
- Diabetes affects the healing of the tendon and reduces the ability to take load.
- Reduced oestrogen hormone can cause loading issues and lead to tendinopathy.
Having said that , the rehab for any tendinopathy is based on loading exercises which are used in a biomechanically correct position to help reduce pain and build the tendon strength back. so don’t get confused. remember injury is caused due to faulty loading and overuse and injury will be resolved with correct loading and appropriate rest.
What are the Risk factors for developing patellar tendinopathy?
For nine risk factors there was some evidence:
- weight,
- body mass index,
- waist-to-hip ratio,
- leg-length difference,
- arch height of the foot,
- quadriceps flexibility,
- hamstring flexibility,
- quadriceps strength and
- vertical jump performance.
Based on the present evidence, reducing body weight, increasing upper-leg flexibility and quadriceps strength and the use of orthotics may be beneficial treatment options. However, it should be stressed that the evidence for the nine identified risk factors was only limited.
Managing Patellar tendinopathy:-
Based on the above classification the treatment is decided.
Strong evidence was found for the use of eccentric training to treat patellar tendinopathy. Moderate evidence was found for conservative treatment (heavy slow resistance training) as an alternative to eccentric training. Moderate evidence suggests that low-intensity pulsed ultrasound treatment did not influence treatment outcomes. Limited evidence was found for surgery, sclerosing injections, and shockwave therapy.(2)
Physical training, and particularly eccentric training, appears to be the treatment of choice for patients suffering from patellar tendinopathy. However, type of exercise, frequency, load, a nd dosage must also be analyzed. Other treatment methods, such as surgical treatment, sclerosing injections, and shockwave therapy, must be investigated further before recommendations can be made regarding their use. Ultrasound can likely be excluded as a treatment for patellar tendinopathy(1)
nd dosage must also be analyzed. Other treatment methods, such as surgical treatment, sclerosing injections, and shockwave therapy, must be investigated further before recommendations can be made regarding their use. Ultrasound can likely be excluded as a treatment for patellar tendinopathy(1)
For proliferative & degenerative causes the research says:-
- the main goals are to reduce pain
- reduce the swelling
- stretching is avoided in this phase
- correction of the biomechanics.
- Loading exercsises once the swelling has subsided.
- Avoid too much rest and inactivity
.
For structural causes the research says:-
The most common inju ry involves acute complete disruption of the tendon with subsequent dysfunction of the extensor mechanism. In this setting, surgical repair is the treatment of choice. In general, repair should be performed as soon as possible after the injury to limit the degree of quadriceps atrophy and prevent any contractures that might make the procedure more difficult.
ry involves acute complete disruption of the tendon with subsequent dysfunction of the extensor mechanism. In this setting, surgical repair is the treatment of choice. In general, repair should be performed as soon as possible after the injury to limit the degree of quadriceps atrophy and prevent any contractures that might make the procedure more difficult.
Regardless of the timing, repair or reconstruction is still the optimal treatment in a patient who has sustained a patellar tendon tear with subsequent patella alta and extensor mechanism dysfunction.
In some situations, a partial tear of the patellar tendon may occur. The patient may be able to maintain full, active extension and normal patellar height. This individual can potentially be treated nonoperatively with immobilization until the tendon has healed. However, one must be certain that the tear is, in fact, partial before initiating this program. Magnetic resonance imaging (MRI) may be useful in this situation(5)
At Physiocure our management is based on the research evidence available. Try these beginner level knee rehabilitation exercises for your patellar tendinpathy , they will definitely help!!
References:-
- Treatment of patellar tendinopathy—a systematic review of randomized controlled trials- Maria E. H. Larsson, Ingela Käll, Katarina Nilsson-Helande- Knee Surgery, Sports Traumatology, Arthroscopy- August 2012
- Risk factors for patellar tendinopathy: a systematic review of the literature- Henk van der Worp1, Mathijs van Ark1, Saskia Roerink2, Gert-Jan Pepping2, Inge van den Akker-Scheek1, Johannes Zwerver1
- Patellar Tendinopathy Sports Health. 2015 Sep; 7(5): 415–420. – Aaron Schwartz, MD,*†Jonathan N. Watson, MD,† and Mark R. Hutchinson, MD† https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4547110/
- The location of pathology in patellar tendinopathy abstracts from the 2nd international scientific tendinopathy symposium (vancouver, 2012)- J d rees⇓, j houghton, a srikanthan, a west https://bjsm.bmj.com/content/47/9/e2.21
- Patellar Tendon Rupture Treatment & Management- Jan 20, 2017 – Author: Christopher C Annunziata, MD; Chief Editor: Thomas M DeBerardino, MD more…https://emedicine.medscape.com/article/1249472-treatment